JANUARY 10, 2023 | BY CELENA ADLER, CMHPL NEWS

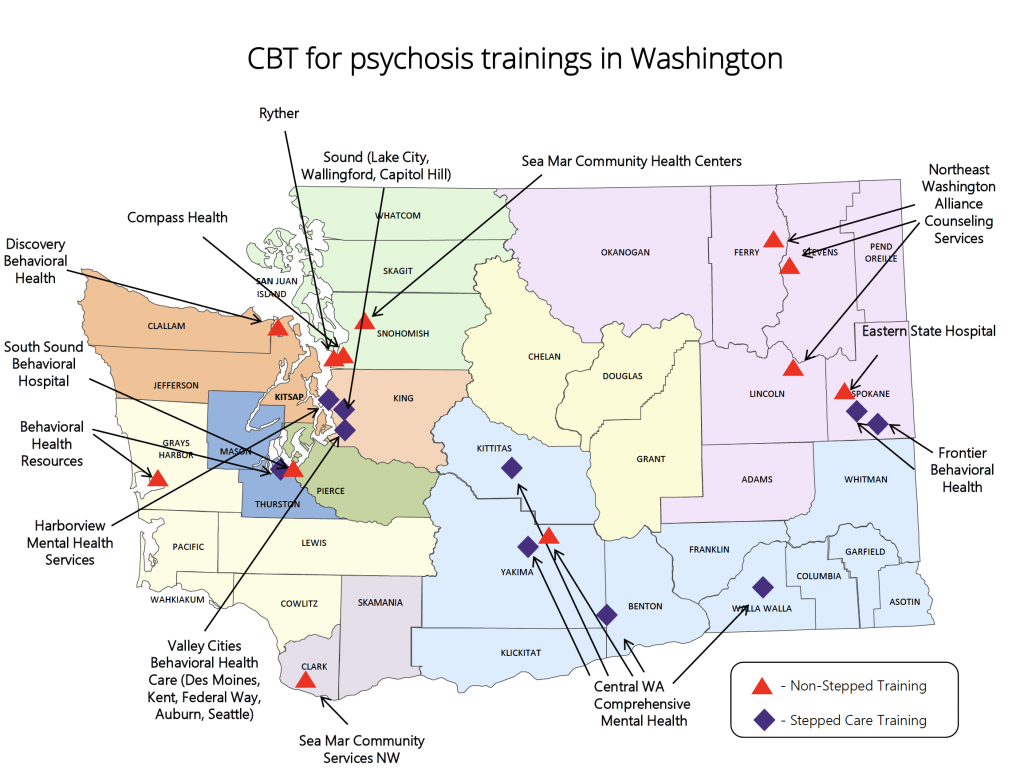
A team at the University of Washington School of Medicine is working to make cognitive behavioral therapy (CBT) for psychosis accessible throughout Washington state.
Psychosis is a symptom involving disconnection with reality, and can include delusions, hallucinations, and disorganized thoughts and speech. Psychosis has several causes, such as mental health conditions like schizophrenia, schizoaffective disorder, and bipolar disorder, as well as other factors like traumatic brain injuries and severe stress. Approximately three percent of people will experience psychosis at some point in their lives.
The efficacy of CBT for psychosis is supported by more than fifty randomized clinical trials conducted over the last thirty years. CBT is effective for treating delusions and hallucinations, reducing the length of hospitalizations, and maintaining gains made in therapy.
In 2022, the UW Center for Mental Health, Policy, and the Law (CMHPL), in collaboration with the UW SPIRIT Lab, launched a CBT Care Pathway demonstration project in Washington. The goal of the CBT Care Pathway is that patients receive CBT while hospitalized, as well as after discharge, ensuring continuity of care. The project is among the first state-funded efforts to provide CBT to patients with serious mental illness throughout their transition from inpatient to outpatient care.
Although the CBT Care Pathway is appropriate for any individual receiving inpatient care for a serious mental illness, the project prioritizes individuals who are involuntarily committed for 90 or 180 days.
“Any time someone is involuntarily hospitalized, it is even more important that we are providing the highest quality care to those patients, so that we can expedite their discharge and reinstate their civil liberties,” explained Dr. Sarah Kopelovich, associate professor in the UW Department of Psychiatry and Behavioral Sciences and CMHPL and SPIRIT Lab core faculty member.
South Sound Behavioral Hospital was one of the early adopters of this new model, receiving training from the UW and implementing CBT for psychosis groups in spring of 2022. Hospital staff have been impressed with how the program has supported their patients’ recovery.
“At first, I was skeptical that cognitive behavioral therapy would resonate with individuals with long-term schizophrenia, schizoaffective disorder, and bipolar disorder,” said Timothy Miller, program director at South Sound Behavioral Hospital. “But it is one of the best treatment programs that I’ve seen in my thirty-some years. It has worked with these long-term populations, when very little does.”
One long-term patient’s experience with the CBT for psychosis group stood out to hospital staff. The patient had schizophrenia, along with several other conditions, which complicated his treatment. He struggled to determine what was real and frequently exhibited angry verbal outbursts towards staff, who questioned whether he would ever be well enough to be discharged.
Previously, the patient had refused treatment, but Linda McFadden, a program therapist, encouraged him to try out the CBT for psychosis group. When he began to consistently attend the group sessions, his outbursts decreased from 10–15 times per day, to one or two times a week. Because of his dramatic improvement of symptoms, he was discharged from the hospital to an adult family home.
“CBT empowers patients,” shared McFadden, who leads the CBT for psychosis group for long-term patients. “It normalizes talking about what’s really going on and creates tiny changes that some people would measure as not good enough. But patients are doing their best, showing up, and incorporating it into their lives. To me, that is success.”
The CBT for psychosis program supported McFadden to tailor treatment to each participant, considering factors like their cultural background, religion, gender, and additional diagnoses.
Dr. Kopelovich hopes that one day, CBT for psychosis will be as readily available as medication. “Medication has been a total game changer in the treatment of schizophrenia and other psychotic disorders, and we know medication works best when combined with talk therapies like cognitive behavioral therapy.”
McFadden highly recommended that other mental health professionals receive training in CBT for psychosis. “In our field we are quite aware of CBT, but sometimes we feel powerless to help patients with schizoaffective disorder and schizophrenia. The training showed me to slow down and meet patients where they are in their own illness and understanding. It’s been positive for them to normalize their experiences and develop coping skills.”
Dr. Kopelovich’s CBT Care Pathway team at the UW includes Rachel Brian, Mel Labelle III, Jeffery Roskelley, Shannon Stewart, and Wenqi Zhang.
This project is funded by the Washington State Healthcare Authority. Additional philanthropic support was made possible through the Professorship of Cognitive Behavioral Therapy for Psychosis, conferred to Dr. Kopelovich in 2017.